Abstract

Background: The presence of peripheral blasts (PB) is a negative prognostic factor in patients (pts) with primary and secondary myelofibrosis (PMF/SMF) and PB ≥4% was associated with a particularly unfavorable prognosis (Masarova L et al, Cancer 2020). Ruxolitinib (RUX) is the JAK1/2 inhibitor most used for treatment of MF-related splenomegaly and symptoms. Its role has not been assessed in correlation with PB.
Aims: To evaluate the impact of PB percentage on RUX efficacy and prognosis
Methods: After IRB approval, the "RUX-MF" retrospective study collected 804 RUX-treated chronic-phase (CP, defined as PB <10%) pts in 26 Hematology Centers. In 794 pts, PB count was evaluated by morphology at RUX start and correlated with treatment success and outcome. Risk category was assessed according to DIPSS (Passamonti F et al, Blood. 2010). Spleen (SR) and symptoms (SyR) response were assessed using IWG-MRT criteria (Tefferi A et al, Blood. 2013).
Comparisons of quantitative variables between the 3 groups were carried out by Kruskal-Wallis and Dunn's tests while association between categorical variables was tested by the χ2 test. Variables significantly associated to RUX stop/leukemic transformation (LT)/overall survival (OS) in univariate analysis (Log-rank test) were considered for multivariable analyses, carried out using the Cox regression model, with evaluation of the model's performance in terms of goodness of fit.
Results: Pts were categorized according to PB at RUX start: PB-0 (no PB; n. 487, 61.3%), PB-5 (PB 1-5%; n. 283, 35.8%), and PB-9 (PB 6-9%; n. 24, 2.9%).
Pts characteristics at RUX start were: median age 68.1y (24-89); males 58.1%; PMF 52.5%; JAK2, CALR and MPL mutated: 80.5%, 13.1% and 2% (4.4% triple negative), high DIPSS: 7.6%; PLT<100/WBC >25 x10 9/l: 10.8%/16.4%; spleen length ≥10 cm: 47.8%, TSS ≥20: 60.6%; ≥1/≥2 high-risk mutation (HMR): 69/18 out of 167 evaluable (41.3%/10.8%); fibrosis grade ≥2: 77.9%; starting/cumulative RUX dose ≥15 mg BID: 61.4%/52.6%.
Higher PB count was associated to high DIPSS risk (PB-0: 1.9%, PB-5: 16.2%, PB-9: 21.7%, p<0.001), PLT<100 x10 9/l (PB-0: 17.6%, PB-5: 15.1%, PB-9: 26.1%, p<0.001), fibrosis grade ≥2 (PB-0: 73.3%, PB-5: 84.2%, PB-9: 100%, p<0.001), spleen length ≥10 cm (PB-0: 43%, PB-5: 55.1%, PB-9: 59.1%, p=0.003).
At 3 and 6 mos, 26.9% and 30.4% of evaluable pts achieved a SR, while 59.7% and 68.1% were in SyR, respectively. At 3 mos, SR (PB-0: 31.8%, PB-5: 20.6%, PB-9: 10%, p=0.001) and SyR (PB-0: 62.9%, PB-5: 55.5%, PB-9: 36.8%, p=0.02) were less frequently achieved by PB-5 and PB-9 pts compared to PB-0 pts. This association remained significant for SR at 6 mos (PB-0: 35%, PB-5: 23.9%, PB-9: 14.3%, p=0.006) and for both SR (p=0.003) and SyR (p=0.01) at any time.
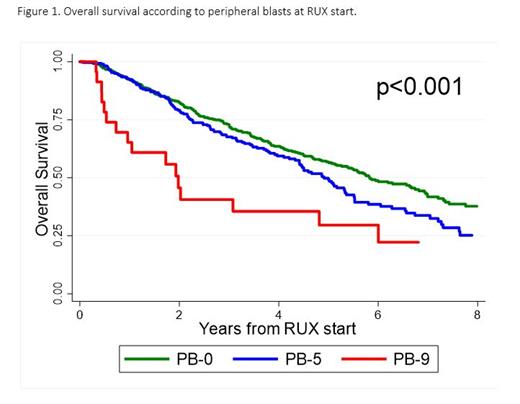
After a median RUX exposure of 1.5 y (0.1-8.9), 491 (61.8%) pts stopped RUX, 110 (13.9%) had a LT and 365 (46%) died. In univariate analysis, at 2y PB-9 pts had higher rates of RUX stop (73.9% vs 40.8% and 34.3% in PB-5 and PB-0 pts, log-rank p<0.001) and LT (38.5% vs 10.2% and 6.2% in PB-5 and PB-0 pts, log-rank p=0.003). Median survival times of PB-0, PB-5 and PB-9 patients were 5.8, 4.9 and 2 years, respectively (log-rank p<0.001) (Figure 1).
In multivariable analysis, PB-9 pts confirmed their association with: 1) RUX stop (HR 3.74, 95%CI 1.51-3.70, p<0.001), with TSS>20 (HR 1.66, 95%CI 1.05-2.61, p=0.03), and HMR≥2 (HR 2.69, 95%CI 1.26-4.47, p=0.007); 2) LT (HR 3.71, 95%CI 1.71-8.04, p<0.001), with HMR≥2 (HR 7.10, 95%CI 2.28-22.1, p<0.001); 3) OS (HR 2.40, 95%CI 1.60-3.60, p<0.001), with age≥65 (HR 2.31, 95%CI 1.17-4.57, p=0.02) and HMR≥2 (HR 3.21, 95%CI 1.67-6.20, p<0.001). Unfavorable association with LT and OS was confirmed also in patients with HMR≥1.
Conclusions: CP-MF pts with PB>5% have a worse response to RUX and a worse outcome. Personalized approaches beyond RUX monotherapy may be useful in this context. Further clinical trials evaluating combination strategies and new drugs are required.
Palandri: Novartis: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; AOP: Membership on an entity's Board of Directors or advisory committees; Sierra Oncology: Membership on an entity's Board of Directors or advisory committees; CTI: Consultancy. Abruzzese: Bristol Myers Squibb: Consultancy, Honoraria; Incyte: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria. Iurlo: Bristol Myers Squibb: Speakers Bureau; Pfizer: Speakers Bureau; Novartis: Speakers Bureau; Incyte: Speakers Bureau. Bonifacio: Bristol Myers Squibb: Honoraria; Novartis: Honoraria; Pfizer: Honoraria; Amgen: Honoraria. Cuneo: AbbVie: Consultancy, Speakers Bureau; AstraZeneca: Consultancy, Speakers Bureau; Janssen: Consultancy, Speakers Bureau; Gilead: Consultancy, Speakers Bureau. Pane: AbbVie; Amgen; Novartis: Other: Travel, accommodation, expenses; Novartis Pharma SAS;: Research Funding; AbbVie; Amgen; Novartis, GSK , Incyte: Consultancy; AbbVie; Amgen; Novartis, GSK, Incyte: Speakers Bureau. Lemoli: Celgene: Other: Support for attending meetings and/or travel; Jazz, Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; AbbVie, Daiichi Sankyo, Servier: Honoraria, Speakers Bureau. Cavo: Bristol-Myers Squib: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Honoraria; Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: TRAVEL, ACCOMMODATIONS, EXPENSES, Speakers Bureau; Adaptive Biotechnologies: Consultancy, Honoraria; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Travel Accommodations, Speakers Bureau; GlaxoSmithKline: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; AbbVie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Breccia: Novartis: Honoraria; Pfizer: Honoraria; Incyte: Honoraria; Bristol Myers Squibb/Celgene: Honoraria; Abbvie: Honoraria.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal